If you have diabetes, your feet need extra care. A small cut or blister can quickly turn into a serious wound. Understanding how to treat diabetic foot ulcers could make the difference between complete healing and serious problems.
One in three people with diabetes will get a foot ulcer at some point. Without proper care, these wounds can lead to bad infections and, in serious cases, amputation. But here’s the good news: with the right treatment, most diabetic foot ulcers heal completely.
What Is a Diabetic Foot Ulcer?
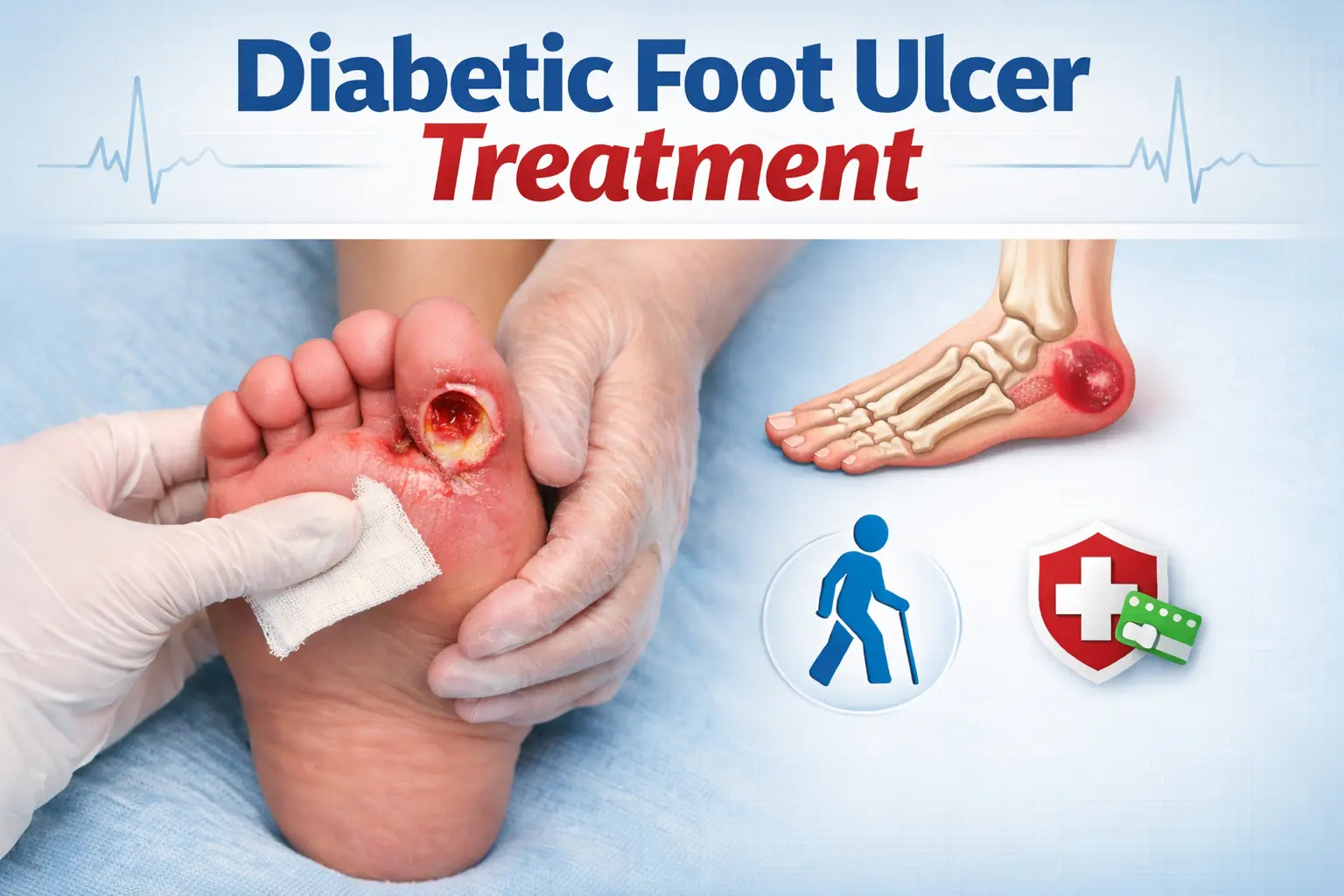
A diabetic foot ulcer is an open sore that usually appears on the bottom of your foot or around your toes. These aren’t regular sores—they go deep through the skin, sometimes reaching the tendons or bones underneath.
The dangerous part? Many people don’t notice them until they’re already serious. Diabetic nerve damage reduces sensation in your feet, so you lose your body’s natural warning system. A small stone in your shoe or a blister from new shoes can quietly turn into a serious wound without you feeling any pain.
Why Do Diabetic Patients Develop Ulcers
Several diabetes-related problems create the perfect conditions for foot ulcers.
– High blood sugar damages nerves over time, reducing pain sensation, so you might walk on an injury for days without knowing.
– Diabetes also reduces blood flow to your feet, meaning less oxygen and fewer nutrients reach damaged tissue to help it heal.
– Foot problems such as bunions or hammertoes create pressure points where skin rubs repeatedly.
Understanding these risk factors explains why diabetic foot ulcer treatment must begin immediately, before minor wounds become major complications.
How to Treat Diabetic Foot Ulcers
Good diabetic foot ulcer treatment needs several approaches working together. Here’s what actually works.
Professional Wound Check and Debridement
This treatment begins with a complete wound check. The podiatrist looks at how deep the ulcer is, its size, location, and whether it’s infected.
Debridement: Removing dead or infected tissue is the essential first step. Dead tissue creates a breeding ground for bacteria and stops healthy skin from growing back.
The podiatrist uses special surgical tools to carefully remove this damaged tissue, creating a clean wound where healthy cells can grow. This usually doesn’t hurt because of nerve damage and may need to be done again at follow-up visits as the wound gets better.
Offloading: Keeping Pressure Off the Wound
This is one of the most important yet often forgotten parts of diabetes podiatry.
Think of it this way: every step on an open wound stops it from healing. Offloading means completely removing weight and pressure from the ulcer so tissue can repair itself properly.
Ways to offload include:
- Special casts that keep the foot still
- Diabetic boots with removable sections
- Custom shoe inserts designed to move weight away from the ulcer
- Protective padding around the wound
- Crutches or wheelchairs for severe cases
Research shows that patients who properly offload their ulcers heal much faster than those who don’t.
Choosing the Right Bandage
What’s the best dressing for diabetic foot ulcers? It depends completely on your wound. Modern wound care goes far beyond simple bandages:
- Hydrocolloid dressings keep the right moisture level for shallow ulcers with little drainage
- Foam dressings absorb extra fluid while cushioning deeper wounds
- Antimicrobial dressings with silver or iodine actively fight bacteria when infection is present
- Calcium alginate dressings handle heavily draining wounds and help with clotting
- Hydrogel dressings add moisture to dry wounds
- Growth factor dressings release proteins that help tissue grow back
- Bioengineered skin substitutes provide a framework for new skin growth
The podiatrist picks and changes dressings based on wound depth, how much it drains, infection status, and healing progress. What works in week one might change as your ulcer gets better.
Fighting Infection with Antibiotics
Infection turns a manageable ulcer into an emergency.
Warning signs include:
- Redness spreading beyond the wound edges
- Increased warmth
- Thick or coloured drainage
- Bad smell
- Fever or chills
- Unstable blood sugar levels
When an infection develops, the podiatrist takes a sample from the wound to identify the specific bacteria. This allows them to choose the right antibiotic.
Treatment includes:
- Antibiotic creams applied directly to the wound
- Oral antibiotics for mild to moderate infections
- IV antibiotics for severe infections, sometimes requiring a hospital stay
- Long-term treatment for deep bone infections
Early infection treatment stops bacteria from spreading deeper into your foot and possibly into your bloodstream.
Blood Sugar Control: The Foundation of Healing
Here’s an uncomfortable truth: even the best wound care fails if blood sugar stays high. If you’re wondering what slows down diabetic wound healing? High glucose tops the list.
High blood sugar hurts healing by:
- Weakening white blood cells that fight infection
- Damaging blood vessels and limiting nutrient delivery
- Interfering with collagen production needed for skin strength
- Reducing oxygen supply to the wound
- Creating an environment where bacteria grow easily
Keeping blood glucose in your target range isn’t just good diabetes management—it’s active wound treatment. Every point you lower your HbA1c improves your ability to heal.
Advanced Diabetic Foot Ulcer Treatment Options
For stubborn ulcers that don’t respond to regular treatment, advanced therapies include:
- Negative Pressure Wound Therapy: Uses controlled suction to remove extra fluid, reduce swelling, and increase blood flow to the wound area.
- Hyperbaric Oxygen Therapy: Delivers concentrated oxygen under pressure, dramatically increasing oxygen levels in damaged tissue. This fights certain bacteria and helps form new blood vessels.
- Platelet-Rich Plasma (PRP): Concentrates healing factors from your own blood and applies them directly to the wound to speed up tissue repair.
- Electrical Stimulation: Uses gentle electrical currents to promote healing at the cell level.
These advanced options are usually saved for ulcers that haven’t improved after 4-6 weeks of standard treatment.
Does Honey Heal a Wound Faster?
Medical-grade honey shows promise for diabetic wounds. Its antibacterial properties fight resistant bacteria, reduce swelling, and keep proper wound moisture. Studies suggest it can speed up healing when used correctly.
However, only sterile, medical-grade honey designed for wound care should be used—regular kitchen honey may contain bacteria that can worsen the infection. Honey works best alongside professional treatment, not as a replacement. Always ask your podiatrist before trying it.
Can Diabetes Cause Toe Swelling?
Yes. Diabetes causes swelling through infection, poor circulation, fluid buildup, or medication side effects. If you notice ongoing swelling with redness, warmth, or an existing ulcer, get immediate medical help. Swelling often signals an infection that needs urgent care.
How to Heal a Foot Ulcer Quickly?
While there’s no instant cure, you can help heal by:
- Going to all appointments
- Following offloading instructions carefully
- Keeping excellent blood sugar control
- Keeping the wound clean and properly dressed
- Checking your feet daily
- Eating enough protein
- Avoiding smoking
- Drinking plenty of water
Most diabetic foot ulcers heal within six to twelve weeks with proper treatment, though severe cases may take several months.
Your Best Treatment is Prevention
The best diabetic foot ulcer treatment is prevention.
Make daily foot checks routine:
- Look for cuts, blisters, redness, or swelling using a mirror for hard-to-see areas
- Wash feet daily with lukewarm water and dry completely, especially between toes
- Use lotion to prevent cracking, but skip the areas between toes
- Trim toenails straight across or have a podiatrist do it
- Never walk barefoot, even indoors
- Check shoes before wearing them for objects or rough seams
- Wear properly fitted shoes—too tight creates pressure points, too loose causes rubbing
When to Get Podiatric Help
Never take a “wait and see” approach with diabetic foot wounds.
Get immediate care if you:
- Find any skin break
- Notice drainage
- Detect a bad smell
- See redness or warmth
- See blackened tissue
- Have a fever with foot symptoms
Early care dramatically improves results.
Expert Diabetic Foot Care You Can Trust
Managing diabetic foot ulcers takes specialised care and close monitoring. At Sydney Podiatry, we understand the challenges diabetes can place on your foot health and provide focused, personalised treatment to support healing and prevention.
As your trusted Sydney Podiatrist, we aim to keep you mobile through proactive care. Whether you’re dealing with an active ulcer or want to prevent foot problems, our experienced team provides the expert attention your feet deserve.
Contact Sydney Podiatry today to schedule a complete diabetic foot assessment at our Double Bay, Drummoyne, or Moree clinic—whichever is most convenient for you.