🩺 Medically Reviewed by Licensed Podiatry Experts
Flat feet, also known as fallen arches or pes planus, occur when the arches of your feet collapse, causing the entire sole to make contact with the ground. This can affect foot biomechanics, posture, gait, and weight distribution, sometimes resulting in pain or fatigue in the feet, ankles, knees, hips, or lower back.
Flat feet are common and often manageable with proper assessment, footwear, strengthening exercises, orthotics, and lifestyle adjustments. This guide provides evidence-based information, including causes, symptoms, evaluation methods, treatments, home remedies, and prevention strategies.
What Are Flat Feet?
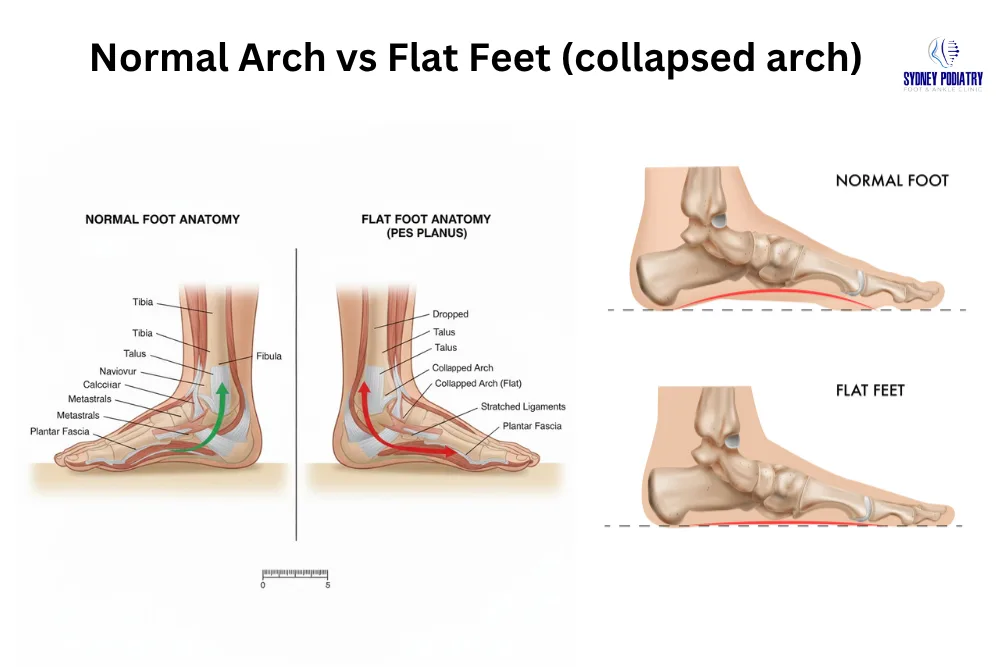
Flat feet occur when the medial arch collapses, making the entire sole of the foot touch the ground. There are two main types:
-
Flexible Flat Feet: The arch is present when not bearing weight but collapses when standing. Often asymptomatic but can lead to pain if unaddressed.
-
Rigid Flat Feet: The arch is permanently flat, sometimes associated with structural issues or previous injury.
Quick Insight
Most flat feet do not require surgery. With targeted exercises, orthotics, and proper footwear, many individuals maintain pain-free mobility.
Types of Flat Feet
Flat feet can present in different forms depending on arch flexibility, bone structure, and underlying causes. Understanding the type is essential for choosing the most effective treatment.
1. Flexible Flat Feet
This is the most common type. The arch appears normal when not bearing weight but collapses during standing or walking. Flexible flat feet often begin in childhood and may remain painless unless the arch-supporting structures weaken over time.
2. Rigid Flat Feet
In this type, the arch remains flat regardless of weight-bearing. It is usually associated with structural abnormalities, previous trauma, arthritis, or congenital conditions. Rigid flat feet typically cause reduced motion in the foot and may lead to ongoing discomfort.
3. Adult-Acquired Flatfoot (AAFD)
This condition develops gradually, most commonly due to posterior tibial tendon dysfunction (PTTD). It often results in progressive arch collapse, ankle instability, and pain along the inside of the foot.
4. Pediatric Flat Feet
Children may naturally have flat feet due to immature arch development. Most resolve with age, but persistent cases—especially those with rigid deformity or functional limitation—should be evaluated by a podiatrist.
Symptoms of Flat Feet
Common signs include:
-
Pain or swelling in the arch, heel, or ankle
-
Feet feeling tired or stiff after long periods of standing
-
Difficulty standing on tiptoes
-
Worn-out shoe edges on the inside
-
Knee, hip, or lower-back discomfort due to misalignment
-
Overpronation: excessive inward rolling of the foot during walking
Causes of Flat Feet
Flat feet may develop due to genetic, structural, or lifestyle factors:
-
Genetic predisposition: Often inherited from parents
-
Foot or ankle injuries: Trauma affecting tendons or ligaments
-
Posterior tibial tendon dysfunction (PTTD): Weakness or injury of the tendon supporting the arch
-
Arthritis or inflammation: Degenerative changes weakening foot structures
-
Obesity: Excessive weight increases arch stress
-
Aging: Natural weakening of tendons and ligaments
-
Neurological or muscular disorders: Affect foot mechanics
-
Tarsal coalition: Abnormal bone connection in children/teens
-
Ligament laxity / hypermobility: Overly flexible connective tissue
Risk Factors for Flat Feet
Several factors increase the likelihood of developing flat feet or experiencing related symptoms:
-
Genetics: Family history of flat arches or hypermobility
-
High body weight: Increased pressure weakens arch-supporting tissues
-
Prolonged standing: Jobs requiring long hours on the feet strain arch structures
-
High-impact sports: Overloads the posterior tibial tendon and arch mechanics
-
Previous injuries: Ankle sprains, fractures, or tendon damage affecting arch stability
-
Improper footwear: Lack of heel and arch support worsens foot mechanics
-
Age-related changes: Tendons and ligaments weaken over time
-
Inflammatory conditions: Conditions like rheumatoid arthritis damage soft tissues
Identifying these risk factors early helps guide prevention and treatment strategies effectively.
When to See a Podiatrist
A professional assessment is recommended when flat feet begin to affect movement, cause ongoing pain, or limit daily activities. Seek podiatric evaluation if you experience:
Persistent pain in the arch, heel, ankle, or inner foot
Difficulty standing on tiptoes or reduced foot mobility
Progressive inward rolling (overpronation) while walking
Visible arch collapse over time
Frequent ankle sprains or instability
Foot pain that interferes with work, exercise, or general mobility
Flat feet in children accompanied by stiffness, limping, or activity avoidance
Early intervention prevents complications such as plantar fasciitis, tendon injuries, knee misalignment, and chronic gait-related issues.
Diagnosis: How Flat Feet Are Evaluated
A podiatrist or orthopedic specialist uses multiple methods to determine flat feet type, severity, and underlying causes:
Clinical Assessment
-
Observing foot posture while standing and walking
-
Tiptoe test to evaluate arch flexibility
-
Checking ankle and foot strength
-
Assessing shoe wear patterns
Specialized Tests
-
Gait analysis & pressure mapping
-
Range of motion in subtalar and midfoot joints
-
Arch Height Index & Foot Posture Index (FPI)
Imaging Studies
-
X-ray: Evaluates bone alignment and arthritis
-
MRI: Examines tendon integrity and soft tissue
-
Ultrasound: Useful for tendon injuries
-
CT scan: Detailed bone structure visualization
This assessment differentiates flexible from rigid flat feet, guiding treatment decisions.
Effective Treatments for Flat Feet
1. Orthotic Insoles or Arch Supports
-
Custom or over-the-counter (OTC) orthotics reduce pain and support the arch.
-
Types include EVA devices, medial arch supports, UCBL orthotics, ankle-foot orthoses (AFO) for severe cases.
-
Orthotics do not cure flat feet but can prevent progression and reduce symptoms.
2. Supportive Footwear
Choose shoes with:
-
Firm midsoles
-
Deep heel cups
-
Proper arch support
Avoid:
-
Thin flats or worn-out sneakers
-
Minimalist shoes if experiencing pain
3. Stretching & Strengthening Exercises
Target arch, Achilles tendon, and intrinsic foot muscles.
-
Calf stretches: Reduce Achilles tension
-
Towel curls: Strengthen arch muscles
-
Heel raises: Support posterior tibial tendon
-
Short-foot exercise: Improve arch control
-
Tennis/lacrosse ball roll: Relieve plantar fascia tightness
Include clear illustrations or diagrams for exercises to increase engagement.

4. Physical Therapy
Tailored therapy may include:
-
Balance retraining
-
Gait correction
-
Soft tissue mobilisation
-
Strength protocols for PTTD
5. Weight Management
Maintaining a healthy weight reduces stress on arches and prevents worsening of symptoms.
6. Pain Relief
-
Short-term NSAIDs
-
Ice or cold compress
-
Anti-inflammatory therapies guided by a clinician
7. Surgical Treatment (Severe or Rigid Flat Feet)
Surgery is last resort when conservative care fails:
-
Tendon reconstruction
-
Calcaneal osteotomy (bone realignment)
-
Arthroereisis (support implant for children/teens)
-
Joint fusion (arthrodesis) for severe deformities
Home Remedies for Flat Feet
- Warm compress to relax tight tissues
- Daily foot and calf stretching
- Avoid prolonged barefoot walking
- Use supportive slippers indoors
- Elevate legs after long standing
- Roll feet on a cold water bottle for inflammation
Prevention Tips
Even with genetic predisposition, you can prevent symptoms:
- Maintain a healthy weight
- Choose supportive daily footwear
- Replace running shoes every 400–500 miles
- Stretch calves and arches regularly
- Avoid standing on hard floors for long periods
- Strengthen intrinsic foot muscles
Long-Term Outlook & Prognosis
Most individuals with flat feet can maintain comfortable, active lifestyles with appropriate management. Flexible flat feet often remain stable when supported with footwear, orthotics, and strengthening programs. Adult-acquired flatfoot may progress if untreated, but early intervention significantly slows deterioration and improves joint alignment.
Rigid flat feet, or cases involving severe tendon dysfunction, may require structured rehabilitation and long-term orthotic use to prevent worsening deformity. Surgical reconstruction is effective when conservative care does not provide relief.
Overall, long-term outcomes are favourable when flat feet are addressed early with targeted treatment based on foot mechanics and the underlying cause.
Summary
Flat feet can affect posture, stability, and comfort, but they are often manageable with targeted exercises, orthotics, supportive footwear, and lifestyle strategies. Early assessment can prevent complications such as plantar fasciitis, Achilles tendinopathy, shin splints, knee misalignment, and chronic joint strain.
Persistent pain, swelling, or progressive arch collapse should be assessed by a podiatrist for a personalized treatment plan.
Medically Reviewed & Expert-Validated Foot Health Guidelines
This article has been reviewed for accuracy and clinical alignment by our podiatry team.
- Correct anatomical references: medial arch, posterior tibial tendon, talus, calcaneus, plantar fascia
- Evidence-based assessment methods: gait analysis, arch index, imaging for bone & tendon evaluation
- Clinically approved treatments including orthotics, physiotherapy, strengthening & gait correction
- Accurate surgical information without overstating outcomes
- Red-flag symptoms identified for when podiatric evaluation is essential
Dr. Shannon Hurvitz, Principal Podiatrist — Specialist in biomechanics, sports medicine & minimally invasive procedures.
Dr. Amanda Sourial — Expertise in diabetic foot care, biomechanics, and podiatric injury management.
Dr. Russell Stokes — 30+ years in sports biomechanics & running injury rehabilitation.
Conclusion
Flat feet are common and manageable when addressed early with the right combination of footwear, strengthening exercises, orthotics, and lifestyle adjustments. For persistent discomfort or structural issues, a podiatry assessment ensures a personalised plan based on your foot type, gait mechanics, and long-term mobility. With proper care, most people can enjoy pain-free, active movement and maintain healthy foot function.
FAQ
Flexible flat feet can often improve with exercises, orthotics, and supportive footwear. Rigid flat feet require professional evaluation.
Most flexible flat feet are manageable; untreated rigid flat feet may contribute to joint problems or overuse injuries.
Some flexible flat feet in children resolve naturally; persistent cases should be assessed.
Supportive shoes with firm midsoles, deep heel cups, and arch support are recommended.
Persistent pain, swelling, or difficulty walking warrants evaluation.
Yes, improper alignment from flat feet can affect knees, hips, and lower back.
No — most cases respond to conservative care. Surgery is reserved for severe deformity, significant tendon damage, or chronic pain.


